I once thought I had multiple sclerosis (MS).
Actually, I may still have multiple sclerosis. I really don’t know for sure.
A few months ago, a series of MS disease-awareness pop-ups began showing up on my web browser. They captured my attention because for a while I’d been experiencing a mix of health ailments—the very same ailments the pop-ups were focusing on. This led me to think that maybe my complaints were linked to multiple sclerosis (MS), and that terrified me. But I kept putting off a doctor’s visit. Then, suddenly, my symptoms went away. Was I cured? Unlikely. Were the pop-ups indicative of an underlying disease? I just didn’t know what to think.
At 81qd, we spend our days thinking about how artificial intelligence (AI) and AI analytics technologies can be positive disruptors for diagnosis.
Using AI to Identify Undiagnosed Patients
Today, AI-driven algorithms can help identify undiagnosed patients with rare and difficult-to-diagnose diseases and the health care professionals (HCPs) who are managing them. These undiagnosed patients can be targeted with messaging on search engines, like I was, which can have quite an impact. But message targeting is only the beginning. The full potential of AI to support diagnosis can be far more impactful.
In order to take advantage of its potential, here are a few important considerations:
How to engage both HCPs and patients, appropriately and effectively, without alienating either.
When to engage HCPs and patients and what is the most effective platform to do so.
When pharma company executives hear about the promise of AI for diagnosis, they hope to walk into an HCP office and jump right into a conversation about undiagnosed patients. Good luck with that. This approach has been met with mixed success. Since patients are de-identified, the discussion is necessarily general. A meaningful discussion has to be insightful without being judgmental, which is difficult to achieve without specific patient information.
When it comes to engaging with patients, the results have been mixed as well. Patients may, in fact, respond to online messaging, but this depends on how well the call to action motivates them. Some patients may find such messaging offensive, while others may be outright dismissive. Experts in patient conversations understand that effective discussions with patients have to be nuanced and sensitive.
In addition to finding patients, AI that is focused on diagnosis can deliver a disruptive impact in three major areas: awareness, activation, and adoption.
AI-Enhanced Awareness: Accelerating Rare Disease Diagnosis
AI can raise awareness of the clinical journey that undiagnosed patients undergo and can inform HCPs about their demographics, which can expedite the journey.
For example, AI can help HCPs identify which patient types are more likely to have a certain disease. It is true that undiagnosed patients may actually look different than diagnosed patients and are, therefore, not receiving appropriate treatment. It is not that HCPs do not want to treat them; it is that HCPs may assume that certain types of patients, and only those types, can have a particular disease.
For one of our clients, we found that with a disease that was perceived as being predominately male, more than 50% of the undiagnosed patients were actually female. The specialists who were managing these patients were just missing them because they were, in a sense, “hiding in plain sight.”
Our client was able to use this critical information to develop targeted patient profiles for the field force that now included women.
Machine-learning algorithms can be used to mine massive amounts of data to understand the nuances of undiagnosed patients. Historically, we have assumed that undiagnosed patients “look the same” as diagnosed patients. While this may be true for rare diseases, in difficult-to-diagnose, yet highly prevalent diseases, this is often not the case.
Activation Strategies using ai data analytics and hcp targeting
AI data analytics can elucidate the clinical journey for undiagnosed patients. Primary care physicians often treat these patients, but engaging a broad range of these physicians across the country is rarely, if ever, feasible.
AI platforms can be useful in mapping connections among specialties in order to assess which HCP networks to activate, which, in turn, facilitate appropriate diagnoses. AI-based solutions can also support multichannel engagement strategies that target HCPs with content on appropriate diagnosis of rare and other difficult-to-diagnose diseases through field activities, peer-to-peer approaches, or online platforms.
drive Adoption of appropriate clinical therapies
AI can help to drive the adoption of clinically appropriate diagnostic and therapeutic approaches.
Educating clinicians is imperative to help shape treatment approaches. Through peer-to-peer programs, education will foster change in HCP practice behavior.
Who should lead these efforts? The most effective approach is to leverage HCP influence. This is done by engaging with clinicians who have the greatest ability to have an impact on the practice patterns of other clinicians, and who are appropriately diagnosing and managing patients.
The key to success is identifying highest-impact HCPs whose networks include HCPs with significant numbers of undiagnosed patients. These clinical influencers have been shown to be highly effective in driving early diagnosis initiatives for other HCPs within their networks. Clearly, AI technologies are powerful tools that will change the clinical journeys of patients across the country. Today, HCPs, patient groups, AI-focused analytics firms, agencies, and pharma companies are working together to solve important challenges and optimize AI-driven strategies for diagnosis. Appropriate and thoughtful engagement with HCPs and patients can have a significant impact on patient lives.
While AI did a good job by targeting me with MS disease-awareness messages, I really wasn’t activated to do something about it—not just yet, anyway. Maybe when I see my doctor, AI will have already alerted her to the diagnostic approaches that can help determine whether or not I have MS.
This might finally be the right time to find out for sure.
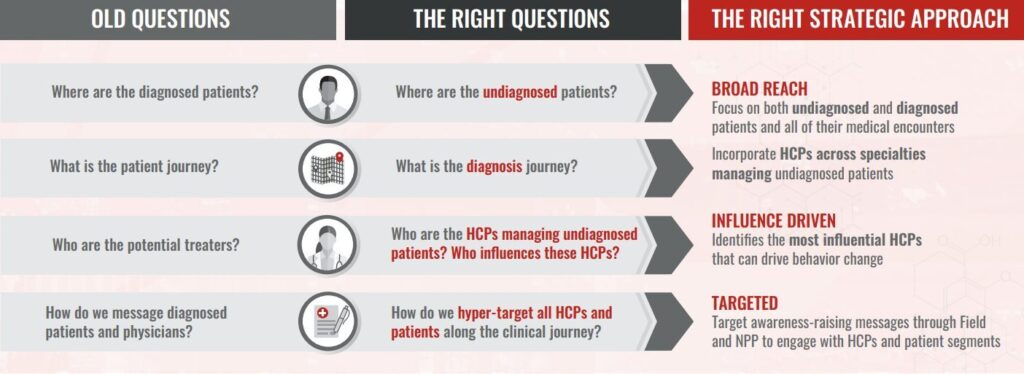
Asking questions to determine strategic outreach for hcps and patients with difficult-to-diagnose or rare diseases